Colon cancer is the third most common cancer in the United States. The American Cancer Society predicts the cancer will cause 51,020 deaths in 2019 alone. However, the overall death rate is starting to drop, thanks to more advanced treatments developed over the last decade.
Detecting colon cancer with blood alone may have been an impossibility just a few years ago, but new developments are starting to suggest otherwise. Can blood tests diagnose colon cancer? A new discovery suggests that it may be possible by identifying circulating tumor cells in the blood.
Overall, colon cancer is still a difficult disease to identify, let alone treat. Multiple testing is often required to reach a conclusive diagnosis. But with a proactive attitude towards screening and testing, there are ways to significantly reduce the risk of developing colon cancer.
Am I At Risk of Colon Cancer?
Studies show that early screening for colon cancer not only reduces its occurrence but also improves a person’s overall mortality (source). Screening is the process of identifying colorectal changes in its earliest forms before significant symptoms even appear.
Screening is especially helpful for individuals who have a higher risk of contracting colon cancer for the following reasons:
- Colon cancer is more commonly diagnosed in adults 50 years old and above. Doctors recommend getting screened for cancer yearly
- People of African-American heritage are at a greater risk of developing colon cancer than other races
- Patients with previous histories of benign colon growths or polyps are still at risk of developing colon cancer in the future
- While colon cancer isn’t hereditary, there are some inherited syndromes that can increase your risk of colon cancer. These include the Lynch Syndrome and familial adenomatous polyposis (FAP) to name a few
- Lifestyle factors such as obesity and heavy alcohol and cigarette consumption
- Patients with inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis
- Type 2 diabetes patients who have a hard time controlling their condition
Polyps and Colon Cancer
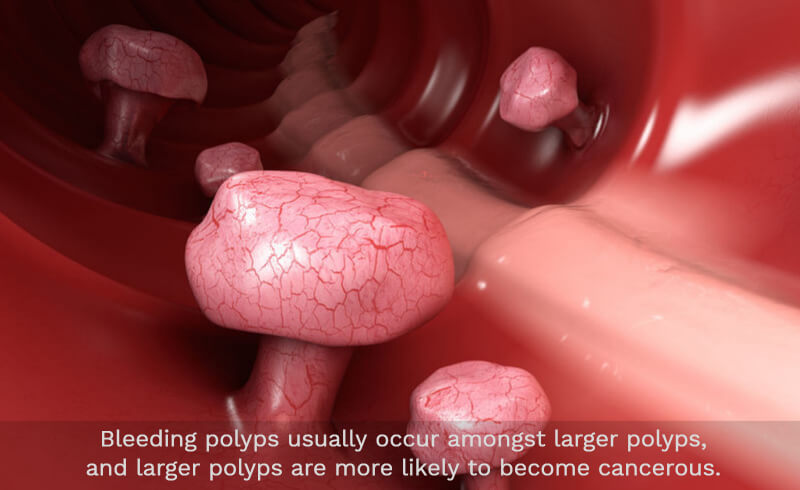
An important part of diagnosing colon cancer revolves around the investigation of existing colon polyps in the digestive system. Colon polyps are cell clumps that can be found along the lining of the colon. While most polyps are benign, a small percentage of them are malignant, becoming cancerous over time. On their own, polyps generally do not cause any symptoms, and grow very slowly over time.
Types of Colon Polyps
Polyps can grow in one of two shapes: stalk polyps or flat polyps, also known as pedunculated or sessile.
When a polyp is pedunculated, it grows into a mushroom shape, with a growth projected outwards attached to a long stalk. Polyps that are sessile are more difficult to detect and remove, as they grow flat against the mucous membrane or lining of the colon.
There are five common types of polyps, all of which should be removed during a colonoscopy for thorough testing. Some of them have a higher chance to develop into colon cancer than others. These types include:
- Adenomatous: A majority of polyps in the colon are the adenomatous type, comprising of roughly around 70% of detected polyps. Most malignant or cancerous types of polyps start as adenomatous growths. With regular screening, doctors can discover malignant polyps before they evolve into colon cancer.
- Villous Adenoma: Around 15% of polyps found in the colon are villous adenoma. Though few, they have a higher chance of evolving into cancer compared to other types of polyps. They are difficult to remove from the colon as they are sessile, meaning they are nearly flat along the lining of the colon.
- Hyperplastic: Hyperplastic polyps are small and common, and carry a low risk of becoming cancerous. These are a kind of serrated polyp, but doctors typically test and remove them in case they are cancerous.
- Polyps from inflammatory disorders: When patients have inflammatory bowel disease, they can develop what is known as inflammatory polyps. They are not polyps in the same sense as other kinds of polyps; rather, they are cell clumps that grew as a reaction to the colon’s long-term inflammation. These polyps are benign and have no chance of becoming colon cancer.
- Serrated: Hyperplastic polyps are a type of serrated polyps. However, there are also bigger serrated polyps that have a higher chance of becoming cancerous. While hyperplastic polyps are generally benign, bigger serrated polyps are more likely to be precancerous.
Why Polyps Bleed, and Other Polyp Symptoms
Most polyps display no symptoms, and can exist in the colon for years, if not decades, undetected. However, there are cases when a candidate for colon cancer finds themselves with blood in their stool. This can be caused by a bleeding polyp, which is generally produced by larger growths along the colon lining:
Other symptoms of polyps include:
- Darkening or reddening color of the stool
- Pain in the abdomen, which is caused by large polyps partially blocking the bowel, making it difficult for the stool to pass
- Anemia caused by iron deficiency, as the chronic bleeding in the stool takes away the iron the body needs for proper oxygen transportation in the body
Are Bleeding Polyps Cancerous?
While there is no direct causation between bleeding polyps and developing colon cancer, we can safely say that bleeding polyps usually occur amongst larger polyps, and larger polyps are more likely to become cancerous.
If you believe that blood in your stool or your abdominal pain may be connected to bleeding polyps, then it is best to see your doctor for a colonoscopy.
Bleeding and Bowels: Hemorrhoid or Colon Cancer?
The presence of blood in the stool is commonly perceived as a telling sign of colon cancer. However, this can signal general problems in the rectum which may not necessarily be related to colon cancer. A good example of which is hemorrhoids.
Hemorrhoids VS Colon Cancer: What’s the Difference?
Hemorrhoids are swollen tissues that have formed in the rectal area. These can occur either inside or outside the anus. Hemorrhoids are caused by straining, a low fiber diet, constipation, and aging.
On the other hand, colon cancer is characterized as abnormal growths on the lining of the colon. When cells deviate from their natural grow-divide-die cycle, they can increase in size and even multiply. When left untreated, polyps can evolve into cancer.
Colon cancer also invades nearby lymph nodes. When blood from the intestine is carried to the liver, colon cancer may spread to the liver once it has targeted nearby lymph nodes.
Why Is There Blood In the Stool?
Rectal bleeding is a symptom common to both colon cancer and hemorrhoids. In the case of hemorrhoids, bleeding occurs when hard stool presses against the swollen hemorrhoid, causing it to bleed.
Similarly, patients with colon cancer also report rectal bleeding. Cancerous polyps tend to bleed more than healthy tissue, resulting in the presence of blood in the feces.
Unlike colon cancer, discomfort and bleeding usually go away in hemorrhoids cases after a couple of weeks. Symptoms persisting or worsening could be indicative of polyps in your colon.
Other Conditions That Cause Bleeding
Not all bleeding is caused by hemorrhoids or colon cancer. Consider the following possibilities the next time you observe blood in your stool:
- Inflammation from syndromes and diseases. Conditions such as Crohn’s disease, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and ulcerative colitis can all cause blood in the stool.
- Bacteria causing bowel infections. Bacteria such as E.coli, Cholera, and Salmonella, along with other common stomach bugs, can cause bloody diarrhea. Soft bloody stool is usually accompanied by intense abdominal cramps. Pain can only be alleviated through antibiotic treatment.
- Large bowels and constipation. Struggling to pass bowels can lead to uncomfortable anal fissures. Common causes include a low-fiber diet and not drinking enough water. A lack of exercise has also been proven to contribute in uncomfortable bowel movements.
Signs You Have Colon Cancer

Rectal bleeding is not the sole sign of colon cancer. In fact, symptoms exhibited by patients may vary. Below are the most common signs of colon cancer:
- A constant change in bowel movement including diarrhea and constipation
- Change in stool consistency
- Cramping, gas, and other forms of pain
- Consistent and progressive abdominal discomfort
- Fatigue and breathlessness
- Unprecedented weight loss (Check out our post on How to Gain Weight with Colon Cancer)
- Feeling bloated
- Inability to pass gas
The presence of blood in the stool is interpreted as an alarming sign of colon cancer. However, that alone is not a conclusive proof of colon cancer. Doctors usually require further testing to clearly establish the cause of the bleeding.
On the other hand, experiencing abnormal bleeding accompanied with one or more of the symptoms above require urgent medical attention. Various tests are available in order to rule out colon cancer.
Do Colon Cancer Patients Always Experience Bleeding?
Contrary to popular belief, colon cancer patients don’t always experience rectal bleeding. This type of cancer spreads slowly and will not produce symptoms for a long time. Symptoms also vary depending on the location and progression of the disease.
One of the biggest myths surrounding colon cancer is the understanding that patients will inevitably exhibit symptoms. However, Dr. Emina Huang (source) from the University of Michigan Medical School affirms that “…the most common symptom is no symptoms at all”.
This is why tests like the fecal occult blood test (FOBT) exist. It is precisely because not all bleeding is visible to the naked eye. Tests like these look for subtle but significant signs of abnormality in your colon and liver, which can help identify colon cancer at its very early stages.
As discussed above, rectal bleeding may very well be symptomatic of other problems in your gastrointestinal system. Either way, we recommend getting screened in order to eliminate the possibilities of colon cancer.
Bright Red Blood: A Sign of Colon Cancer?
Blood in the stool is commonly a sign of hemorrhoids, not colon cancer. As the stool passes along, the swollen tissue may obstruct the stool, causing the hemorrhoid to rupture and bleed. The blood is usually bright red in color and watery in consistency.
On the other hand, bleeding from colon cancer is typically described as darker in appearance. Stool ranging from maroon to tar-like can be a sign of colon abnormalities. This is because the blood is produced higher up in the colon and is “less fresh” than one from a hemorrhoid rupture.
Again, it’s impossible to accurately diagnose colon cancer from the color of the stool alone. We recommend a proper examination to really understand your state of health.
Is It Common to See Blood In the Urine?
No. The presence of blood in the urine is usually a sign of bladder cancer, not colon cancer. If you suspect having or have been diagnosed with colon cancer but observe blood in your urine, this might be a sign of further complications not related to your colon.
Bladder cancer can be identified through various urine tests, one of them being cytology. Frequent urination, pain during urination, and the inability to pass urine are all signs of bladder cancer.
The Clue Is In Your Blood
Blood picks up chemicals, cells, and other elements as it flows from one part of the body to the other. Blood work offers clues regarding your general health, providing an insight into abnormal functions in the body.
Colon Cancer and White Blood Cell Count
White blood cells are produced in the bone marrow and are easily detectable in blood tests. A specific type of white blood cell called the neutrophil is responsible for warding off infections and destroying harmful cells.
The normal neutrophil count is 1,000/1 microliter. A deficiency in neutrophils is called neutropenia. This is caused by severe infections that are too invasive.
On the other hand, neutrophil production can also be stalled by the presence of cancer. Cancer treatments can also affect neutrophil count due to radiation exposure. Keeping track of your neutrophil count can help you understand how your body works.
Red Blood Cell Count and Bleeding Polyps
Blood tests look at hemoglobin levels in red blood cells. This protein is responsible for bringing fresh oxygen into the blood and transporting it throughout the body. A dysfunction in red blood cells is called anemia.
Anemic people have symptoms such as:
- Fatigue
- Paleness
- Chest pain
- Dizziness and sporadic headaches
- Difficulty breathing
- Heart palpitations
Anemia is caused by multiple abnormalities, including cancer itself. Bleeding polyps can worsen over time. When this happens, the survival rate of patients with cancer is threatened. Anemia deprives the body of fresh oxygen, which in turn affects the body’s capability to cope with cancer treatments.
Blood Testing and Colon Cancer
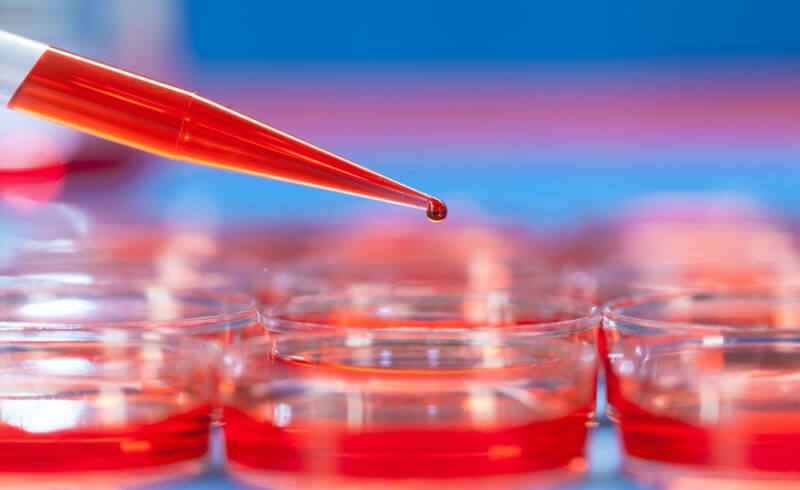
It’s common for those getting screened for colon cancer for the first time to expect a thorough blood test to rule out the possibility of colon cancer. However, blood tests aren’t the be-all and end-all test. Additional examination is required if results come out positive from a blood test.
Can a Blood Test Detect Colon Cancer?
Colon cancer can’t be directly identified from your blood alone. Blood tests are usually supplementary tests performed by doctors to understand your overall health. Trace elements from carcinogens can appear in your blood test results, which inform doctors about abnormalities in your body.
The common blood tests performed to detect colon cancer are:
Fecal occult blood test (FOBT). Occult blood is blood that is invisible to the naked eye. A sample of your stool is studied to check for problems in the digestive tract. Positive results don’t necessarily mean colon cancer; benign tumors, ulcers, and other conditions concerning the digestive tract may also cause results to come back positive.
Carcinoembryonic antigen (CEA). The CEA is less of a test and more of a trace element. Cancerous cells sometimes produce this chemical in the blood. Doctors usually track the level of CEA in a patient’s body over a long period of time. This helps them understand how colon cancer is progressing in the body. Treatment efficacy is also based on long-term CEA levels.
The Future of Blood Testing
As mentioned, blood tests aren’t typically considered as stand-alone methods of diagnosis for colon cancer. However, recent findings suggest otherwise.
New research suggests that blood tests can finally be used to find colon cancer, catching it even in its early stage (source). This experiment was conducted in a hospital in Taoyuan, Taiwan where 620 participants were tested for CTCs or circulating tumor cells.
The blood sample is analyzed with a blood assay called CMX. The results were able to distinguish CTCs present in the blood, which is useful in identifying people with both precancerous polyps and existing colon cancer.
How accurate is this new blood test for colon cancer? The results came back with an 84-88% accuracy, with false positives only coming back at less than 3%. These numbers are significantly better than FOBT, which is the standard method for detecting colon cancer.
Significance and Possible Application
Discoveries like this are pivotal because they allow for earlier detection and treatment. When it comes to most types of cancer, early detection is the key to treating it successfully.
Patients diagnosed with a localized stage colon cancer have a 90% chance of survival within five years (source). That drops to 71% after cancer has spread to neighboring organs and systems. It drops to 14% once it spreads to farther parts of the body.
With technology this accurate, doctors can gain a better insight into the development of colon cancer. More importantly, colon cancer mortality rates will drop significantly in the future, thanks to the possibility of early detection.
For patients, this translates to more affordable and comfortable methods of screening. As lead author doctor Wen-Sy Tsai notes, “There is still some reticence among patients to use stool-based tests or have an invasive exam like colonoscopy to detect colorectal cancer. Our results may point to a solution.” (source)
Other Tests
1. Sigmoidoscopy
A sigmoidoscopy is a close inspection of the sigmoid colon. This is connected to the anus through the rectum. A flexible tube with a light attached at the end is inserted into your anus. The camera attached is used to look for polyps. Sigmoidoscopy has been proven to significantly reduce mortality by detecting polyps in the distal colon.
2. Colonoscopy
A colonoscopy is similar to a sigmoidoscopy in that a small, camera-enabled tube is inserted into your rectum for examination. However, colonoscopies are usually performed to observe the entire colon. Tissue samples may also be taken during a colonoscopy for further study.
3. Virtual Colonoscopy
Virtual colonoscopies don’t involve physical insertion. Also called a computed tomography colonography, this procedure uses a special x-ray machine to examine the colon for polyps. A small of gas is introduced to your colon through the rectum, and CT images are taken to detect polyps.
Preparing For a Fecal Occult Blood Test
Although performed at home, some preparation is necessary for successful testing. Certain medications and foods can affect the results of the FOBT. As such, it’s important to follow common guidelines to ensure accurate results:
- Consult your doctor regarding the special diet. Certain foods affect test results, which is why it’s important to know foods that are permissible to eat. Raw fruits and vegetables are generally a no-go. Red meat such as beef and pork are usually banned by doctors for up to 72 hours before the test because blood in the meat may cause a false positive result
- Citric foods rich in Vitamin C may also alter the test. Stay away from foods and beverages with high vitamin C content
- Certain medication may interfere with the exam. Your doctor will put certain medicines on hold up to 72 hours before the exam
Different Kinds of FOBT
There are two main types of FOBT:
Guaiac Smear Test (gFOBT)
- Collect three different samples from separate bowel movements
- Swab the stool and store it in the given container. Ensure that it doesn’t get in contact with urine or water
- Label your samples, as per the instruction
- Submit your results for testing
Fecal Immunochemical Test (FIT)
- Collect three different samples from separate bowel movements
- A special device will be included in your kit. Use this to collect the sample
- Swab the sample onto a test card, or any container provided on your kit
- Label your samples, as per the instruction
- Submit your results for testing
Remember: Early detection is the best way to fight colon cancer.
Get screened for colon polyps today.
