Colonoscopy side-effects vary from patient to patient, but one particular side-effect is causing discomfort among patients: back pain.
So, is back pain after colonoscopy serious? While uncommon compared to the other side-effects, back pain after a colonoscopy is safe and reported more often than you think. After a colonoscopy, your bowels may still be experiencing soreness, and this discomfort radiates through your body and sometimes reaches the upper or lower back.
In this article we explain why patients experience back pain after a colonoscopy, and how to treat it at home.
Common Colonoscopy Side-Effects
A colonoscopy is a minimally invasive procedure that is routinely performed as a screening method. Because of its minimally invasive nature, patients can expect some common side-effects including:
- Dizziness or lethargy due to anesthesia/sedative
- Stomach cramps
- Irregular bowel movements
- Abdominal pain
- Abdominal distension
- Feeling bloated or full
- Nausea
- Excess gas evidenced by flatulence or burping
- Back pain
These side-effects are experienced by most patients who have undergone a colonoscopy. Expect to feel these symptoms up to 48 hours after your procedure.
When to See a Doctor
Any medical procedure has risks, including a colonoscopy. However, only 2 out of 1,000 procedures result in a complication, making it one of the safest medical procedures.
- Bleeding: Bleeding in the rectum is a tell-tale sign that something is wrong. If you can observe blood in your poop 3-4 days after your colonoscopy, get in touch with your doctor immediately. Bleeding could be a sign of colon perforation.
- Persistent Symptoms: The symptoms outlined above are normal and should be no cause for worry. However, if they remain 3 to 4 days after the procedure and are getting worse with time, it could be a sign that something is wrong.
For instance, cramping in the abdomen is normal after a colonoscopy. But if experienced for extended periods of time, this could point to something more serious such as intestinal blockage, trapped air, or even bowel perforation.
Back Pain Post-Colonoscopy

Back pain is not often listed as a side-effect after a colonoscopy. This is because of two reasons:
- Back pain is usually not reported because it’s uncommon compared to the other side-effects like gassiness, abdominal pain, or temporary constipation
- When patients do experience back pain, they seldom link it back to their colonoscopy and instead find other ways to explain why the back pain exists
As such, it’s not common knowledge that back pain can happen after a colonoscopy. Although common, this side-effect is not so rarified as to raise medical questions.
What does back pain after a colonoscopy feel like?
Anecdotes from patients vary. Some patients experience pain radiating from the upper back to their shoulders, which is more common in patients who have undergone upper endoscopies alongside their colonoscopies.
Most patients who undergo a colonoscopy localize their pain in the lower back. They characterize the pain as numbness, soreness, or pinching. Some patients experience pain on the lower end of the back, near the tailbone, and compare their pain to sciatica pain; while others talk about lower back pain concentrated on the right or left areas.
Is back pain a sign of colon perforation?
In the event of colon or bowel perforation, patients normally experience severe abdominal pain that gets worse or doesn’t subside in a day or two. Back pain is not a sign of colon perforation and is more likely a sign of bowel soreness, which is common and safe.
If you’re experiencing abdominal pain that’s progressively getting worse 2-3 days after your colonoscopy, get in touch with your doctor immediately.
Back Pain After a Colonoscopy: Why It Happens
It can be puzzling to experience back pain after a colonoscopy, precisely because this body part is so far away from the colon. In reality, it still happens, and thankfully it’s not because of colon perforation.
The back pain associated with a colonoscopy is characterized as referred pain. This type of pain is felt in locations other than where the cause is located. For instance, a colonoscopy patient can experience pain at the back, even though the procedure only involved the bowels.
Referred pain is a common condition. For instance, the first signs of a heart attack aren’t localized in the heart. Instead, they can be felt in the teeth, jaws, or more commonly, the arms.
What is Referred Pain?
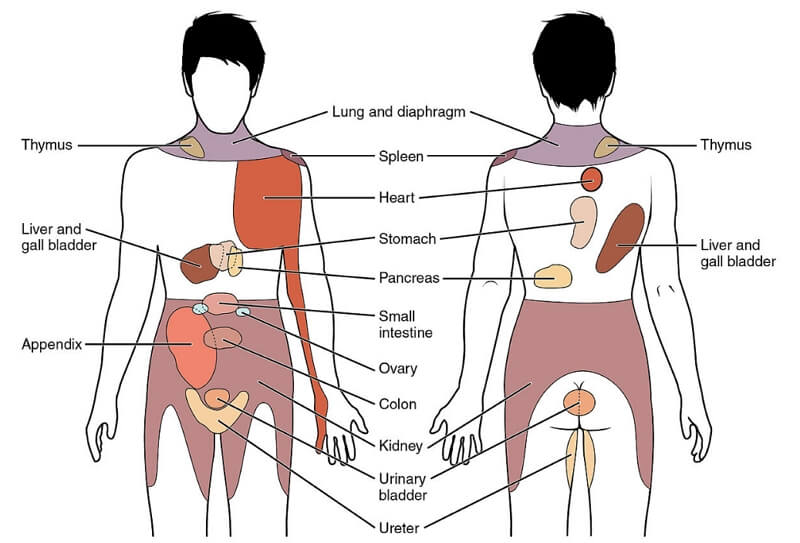
The body houses a network of muscles, nerves, and tissues that communicate with each other. Pain from one location can translate into pain in another location as the body interprets various signals and stimuli and try to convert those into information.
Because the brain is receiving multiple signals at once, neurons may refer to pain “reports” ambiguously, and localize it to a different part of the body, confusing it with the right location of the stimulus.
In the case of colonoscopy patients, the bowels may still be sore from the procedure, causing the body to misinterpret bowel discomfort as generalized back pain. Keep in mind that back pain from colonoscopy is temporary and should disappear as the bowels recover from the procedure.
How to Alleviate Back Pain at Home
Back pain may not be a cause for worry but it’s still uncomfortable and deserves at-home intervention. Here are some things you can do to alleviate your back pain:
- Use a pillow. Provide relief to your back by sleeping with a pillow on your back or on your knees, depending on your stature. Experiment with different pillow positions to give your back the best support and relief.
- Take pain relief medication. Instant pain relief from medication always helps. Over the counter medicine such as ibuprofen are useful in treating back pain. If you’re experiencing severe back pain, ask your doctor if you can have some prescription medication to help soothe the pain.
- Bed rest. Patients are encouraged to take a full rest day the day after their colonoscopy. If you’re experiencing back pain, it’s best to extend your rest day 2-3 days after the procedure to really allow your back to relax.
- Use hot or cold therapy. Ice and heat packs are available commercially. You can use cold packs to help with pain and inflammation. Heat packs are great for encouraging blood flow and pain relief. For post-colonoscopy back pain, it’s a good idea to use both to treat back pain. Apply the cold or hot compress for 20-30 minutes at 2-4 hour intervals.
When to Call a Professional
If your back pain persists 3-4 days after your colonoscopy, get in touch with your doctor to understand the source of your pain. In very rare occasions, you may be recommended to undergo an imaging procedure such as a CT scan in order to rule out the possibility of musculoskeletal damage. Your doctor may prescribe some anti-inflammatory medication to help treat back pain.
Schedule Colonoscopy with Us
At Gastro Center NJ, we give you the proper care to prevent any complications after your colonoscopy. During our procedure, we make sure our patients are properly sedated, comfortable, and safe. Our medical professionals are here to take care of you from start to finish.
Are you experiencing any disconcerting symptoms after your colonoscopy? Get in touch with us today to get a second opinion, and we’ll find ways to alleviate your side-effects and restore you back to your best health.
